Understanding our internal clock to improve health
Why circadian timing matters for health and disease
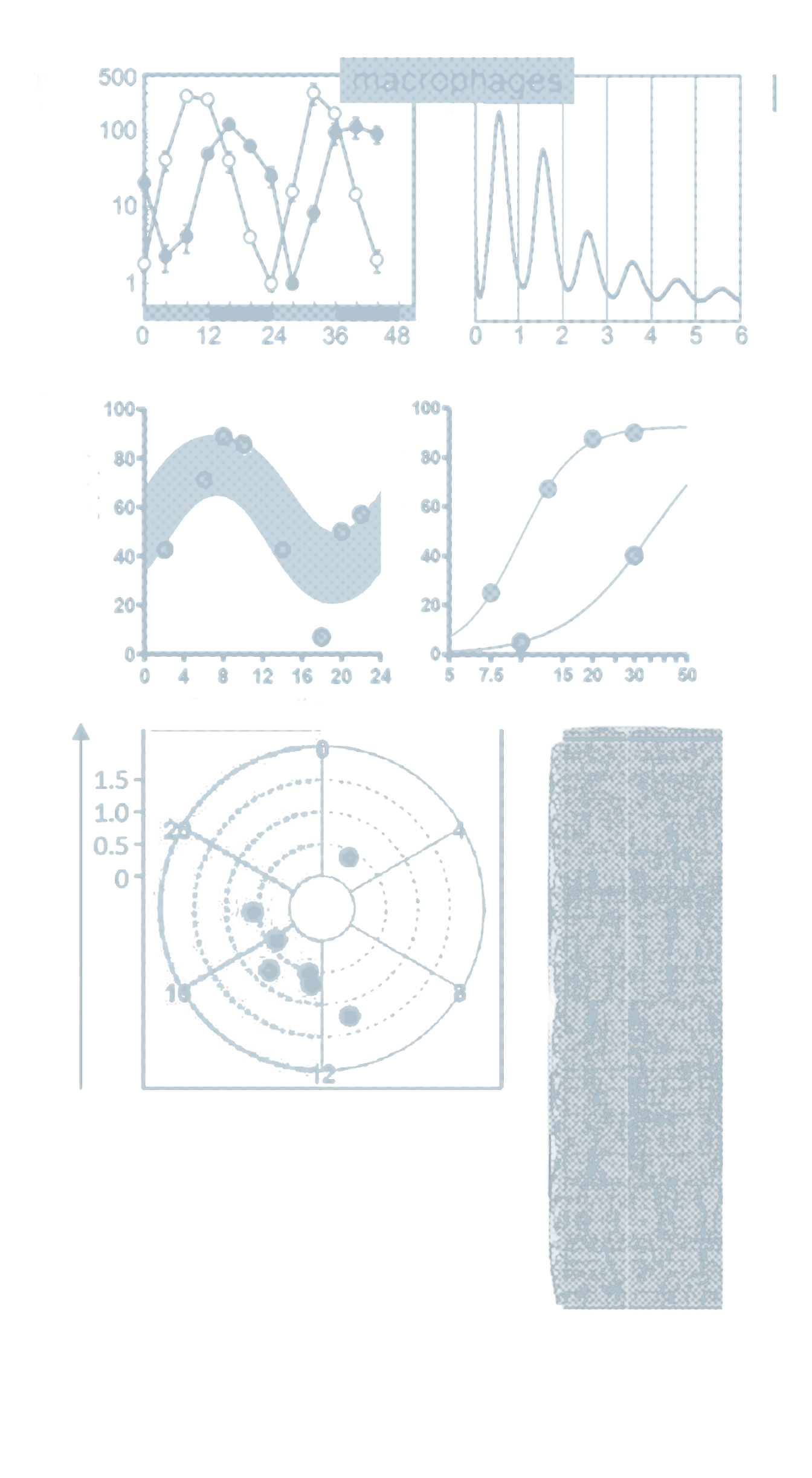
Our internal clock governs fundamental physiological processes throughout the body. When this temporal orchestration is disrupted, disease can arise long before symptoms become apparent. This challenge, however, presents a transformative opportunity: understanding the mechanisms of circadian timing can redefine how we prevent, diagnose, and treat illness.
Our consortium envisions circadian biology as a unifying framework for future medicine. We aim to reveal how disrupted timing drives disease, and to develop strategies to measure ("Detecting"), restore ("Targeting"), and therapeutically harness ("Exploiting") the circadian clock. Through this work, we seek to pave the way toward a future in which medicine is predictive, personalized, and precisely aligned with the body’s endogenous rhythms.
The voices of TRR 418

We are excited to explore the potential of circadian medicine to reshape how health is approached. Our vision is to align medical strategies with the body’s internal clock.
Achim Kramer
Spokesperson

We rely on a solid scientific foundation to understand how timing affects physiology and disease. Together, we uncover mechanisms that guide precise, evidence-based interventions.
Henrik Oster
Deputy Spokesperson

We see daily how disrupted rhythms influence patient recovery and well-being. By addressing and restoring these patterns, we aim to improve care and outcomes.
Claudia Spies
Deputy Spokesperson
Our projects
Our projects translate the principles of circadian medicine into focused research questions. Each project addresses a specific biological system, disease context, or methodological challenge, while contributing to a shared, transdisciplinary effort. Together, they connect mechanistic insight, clinical investigation, and data-driven approaches to advance circadian diagnostics, interventions, and therapies. Explore the projects to see how circadian medicine is studied in practice.

A01
Mechanisms of circadian vaccination responses in humans and mice
Mechanisms of circadian vaccination responses in humans and mice

B02
Circadian desynchronization and epigenetic alteration crosstalk on the development and resolution of metabolic dysfunction-associated steatohepatitis
Circadian desynchronization and epigenetic alteration crosstalk on the development and resolution of metabolic dysfunction-associated steatohepatitis
C01
Individualized data-driven light intervention in intensive care unit patients
Individualized data-driven light intervention in intensive care unit patients
The publications of TRR 418
The publications of TRR 418 present the scientific foundations of the consortium’s work in circadian medicine. They provide detailed insight into experimental, clinical, and data-driven studies that underpin advances in understanding circadian timing in health and disease. Explore our publications to engage with the evidence, methods, and scientific reasoning behind this research.
Time-of-day immunochemotherapy in non-small cell lung cancer: a randomized phase 3 trial
February 2, 2026
•
Nature Medicine
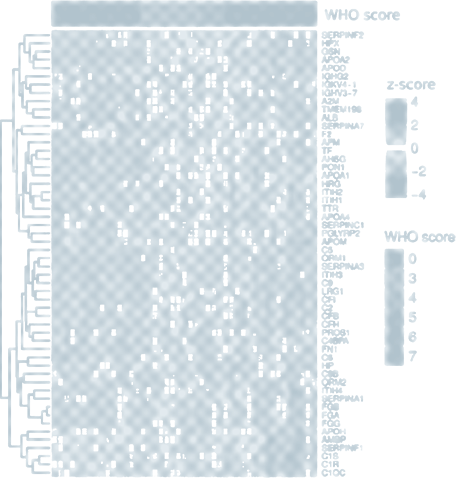
Retrospective studies suggest that early time-of-day (ToD) infusions of immunochemotherapy may improve efficacy. However, prospective randomized controlled trials are needed to validate it. In this randomized phase 3 LungTIME-C01 trial, 210 patients with treatment naive stage IIIC–IV non-small cell lung cancer (NSCLC) lacking driver mutations were randomly assigned in a 1:1 ratio to either an early or late ToD group, defined by the administration of the first four cycles of an anti-PD-1 agent before or after 15:00 h. The primary endpoint was progression-free survival (PFS), while secondary endpoints included overall survival (OS) and objective response rate (ORR). After a median follow-up of 28.7 months, the median PFS was 11.3 months (95% confidence interval (CI) = 9.2–13.4) in the early ToD group and 5.7 months (95% CI = 5.2–6.2) in the late ToD group, corresponding to a hazard ratio (HR) for earlier disease progression of 0.40 (95% CI = 0.29–0.55; P< 0.001). The median OS was 28.0 months (95% CI = not estimable (NE)–NE) in the early ToD group and 16.8 months (95% CI = 13.7–19.9) in the late ToD group, corresponding to an HR of an earlier death of 0.42 (95% CI = 0.29–0.60; P< 0.001). Treatment-related adverse events were consistent with the established safety profile, with no new safety signals observed. No significant differences in immune-related adverse events were observed between the two groups. Over the first four cycles, morning circulating CD8+ T cells increased in the early ToD group, whereas they declined in the late ToD group (P< 0.001). Furthermore, the ratio of activated (CD38+ HLA-DR+) versus exhausted (TIM-3+PD-1+) CD8+ T cells was higher in the early ToD group (P< 0.001) compared with the late ToD group (P< 0.001). In summary, our study indicates that early ToD immunochemotherapy substantially improves PFS and OS and is associated with enhanced antitumor CD8+ T cell characteristics compared with late ToD treatment.
Time-of-day immunochemotherapy in non-small cell lung cancer: a randomized phase 3 trial
February 2, 2026
Retrospective studies suggest that early time-of-day (ToD) infusions of immunochemotherapy may improve efficacy. However, prospective randomized controlled trials are needed to validate it. In this randomized phase 3 LungTIME-C01 trial, 210 patients with treatment naive stage IIIC–IV non-small cell lung cancer (NSCLC) lacking driver mutations were randomly assigned in a 1:1 ratio to either an early or late ToD group, defined by the administration of the first four cycles of an anti-PD-1 agent before or after 15:00 h. The primary endpoint was progression-free survival (PFS), while secondary endpoints included overall survival (OS) and objective response rate (ORR). After a median follow-up of 28.7 months, the median PFS was 11.3 months (95% confidence interval (CI) = 9.2–13.4) in the early ToD group and 5.7 months (95% CI = 5.2–6.2) in the late ToD group, corresponding to a hazard ratio (HR) for earlier disease progression of 0.40 (95% CI = 0.29–0.55; P< 0.001). The median OS was 28.0 months (95% CI = not estimable (NE)–NE) in the early ToD group and 16.8 months (95% CI = 13.7–19.9) in the late ToD group, corresponding to an HR of an earlier death of 0.42 (95% CI = 0.29–0.60; P< 0.001). Treatment-related adverse events were consistent with the established safety profile, with no new safety signals observed. No significant differences in immune-related adverse events were observed between the two groups. Over the first four cycles, morning circulating CD8+ T cells increased in the early ToD group, whereas they declined in the late ToD group (P< 0.001). Furthermore, the ratio of activated (CD38+ HLA-DR+) versus exhausted (TIM-3+PD-1+) CD8+ T cells was higher in the early ToD group (P< 0.001) compared with the late ToD group (P< 0.001). In summary, our study indicates that early ToD immunochemotherapy substantially improves PFS and OS and is associated with enhanced antitumor CD8+ T cell characteristics compared with late ToD treatment.