Unsere innere Uhr verstehen, Gesundheit verbessern
Warum circadiane Rhythmen für Gesundheit und Krankheit entscheidend sind
Unsere innere Uhr steuert grundlegende physiologische Prozesse im gesamten Körper. Gerät diese zeitliche Orchestrierung aus dem Gleichgewicht, können Krankheiten entstehen, häufig lange bevor erste Symptome erkennbar sind. Gleichzeitig eröffnet sich darin eine wegweisende Chance: Ein vertieftes Verständnis der Mechanismen des circadianen Timings kann grundlegend verändern, wie wir Krankheiten vorbeugen, diagnostizieren und behandeln.
Unser Konsortium begreift die circadiane Biologie als ein verbindendes Rahmenkonzept für die Medizin der Zukunft. Wir untersuchen, wie gestörte zeitliche Abläufe zur Krankheitsentstehung beitragen, und entwickeln Strategien, um die innere Uhr zu messen („Detecting“), zu beeinflussen („Targeting“) und therapeutisch zu nutzen („Exploiting“). Damit möchten wir den Weg zu einer Medizin ebnen, die prädiktiv, personalisiert und präzise an den endogenen Rhythmen des Körpers ausgerichtet ist.
Die Stimmen von TRR 418

Wir sehen in der circadianen Medizin ein zentrales Zukunftsfeld, das medizinisches Denken und Handeln neu prägen kann. Unsere Vision ist es, medizinische Strategien mit der inneren Uhr des Körpers zu synchronisieren.
Achim Kramer
Sprecher

Wir stützen uns auf eine solide wissenschaftliche Basis, um zu verstehen, wie zeitliche Abläufe Physiologie und Krankheitsprozesse beeinflussen. Gemeinsam entschlüsseln wir Mechanismen, die präzise, evidenzbasierte Interventionen ermöglichen.
Henrik Oster
Stellvertretender Sprecher

Täglich sehen wir, wie gestörte circadiane Rhythmen Genesung und Wohlbefinden beeinflussen. Durch ihre Wiederherstellung wollen wir Versorgung und Therapieergebnisse verbessern.
Claudia Spies
Stellvertretende Sprecherin
Unsere Projekte
Unsere Projekte übersetzen die Prinzipien der circadianen Medizin in klar definierte Forschungsfragen. Jedes Projekt fokussiert sich auf ein spezifisches biologisches System, einen Krankheitskontext oder eine methodische Herausforderung und trägt zugleich zu einem gemeinsamen, transdisziplinären Ansatz bei. Zusammen verbinden sie mechanistische Erkenntnisse, klinische Forschung und datengetriebene Methoden, um circadiane Diagnostik, Interventionen und Therapien voranzubringen. Entdecken Sie unsere Projekte und erfahren Sie, wie circadiane Medizin in der Praxis erforscht wird.
A01
Mechanismen der circadianen Impfantworten bei Menschen und Mäusen
Mechanismen der circadianen Impfantworten bei Menschen und Mäusen
B02
Circadiane Desynchronisation und epigenetische Veränderung: Wechselwirkungen bei der Entwicklung und Auflösung von mit metabolischer Dysfunktion assoziierter Steatohepatitis
Circadiane Desynchronisation und epigenetische Veränderung: Wechselwirkungen bei der Entwicklung und Auflösung von mit metabolischer Dysfunktion assoziierter Steatohepatitis
C01
Individualisierte datengesteuerte Lichtintervention bei Patienten auf der Intensivstation
Individualisierte datengesteuerte Lichtintervention bei Patienten auf der Intensivstation
Die Publikationen von TRR 418
Die Publikationen von TRR 418 bilden die wissenschaftliche Grundlage der Arbeiten des Konsortiums in der circadianen Medizin. Sie geben vertiefte Einblicke in experimentelle, klinische und datenbasierte Studien, die unser Verständnis der circadianen Zeitsteuerung in Gesundheit und Krankheit voranbringen. Entdecken Sie unsere Publikationen und gewinnen Sie Einblick in die Evidenz, Methoden und wissenschaftlichen Konzepte hinter dieser Forschung.
Time-of-day immunochemotherapy in non-small cell lung cancer: a randomized phase 3 trial
February 2, 2026
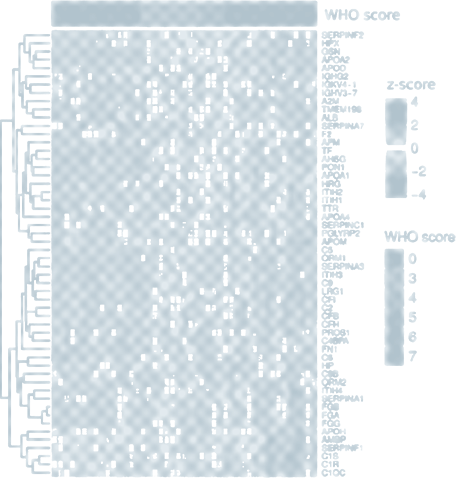
Retrospective studies suggest that early time-of-day (ToD) infusions of immunochemotherapy may improve efficacy. However, prospective randomized controlled trials are needed to validate it. In this randomized phase 3 LungTIME-C01 trial, 210 patients with treatment naive stage IIIC–IV non-small cell lung cancer (NSCLC) lacking driver mutations were randomly assigned in a 1:1 ratio to either an early or late ToD group, defined by the administration of the first four cycles of an anti-PD-1 agent before or after 15:00 h. The primary endpoint was progression-free survival (PFS), while secondary endpoints included overall survival (OS) and objective response rate (ORR). After a median follow-up of 28.7 months, the median PFS was 11.3 months (95% confidence interval (CI) = 9.2–13.4) in the early ToD group and 5.7 months (95% CI = 5.2–6.2) in the late ToD group, corresponding to a hazard ratio (HR) for earlier disease progression of 0.40 (95% CI = 0.29–0.55; P< 0.001). The median OS was 28.0 months (95% CI = not estimable (NE)–NE) in the early ToD group and 16.8 months (95% CI = 13.7–19.9) in the late ToD group, corresponding to an HR of an earlier death of 0.42 (95% CI = 0.29–0.60; P< 0.001). Treatment-related adverse events were consistent with the established safety profile, with no new safety signals observed. No significant differences in immune-related adverse events were observed between the two groups. Over the first four cycles, morning circulating CD8+ T cells increased in the early ToD group, whereas they declined in the late ToD group (P< 0.001). Furthermore, the ratio of activated (CD38+ HLA-DR+) versus exhausted (TIM-3+PD-1+) CD8+ T cells was higher in the early ToD group (P< 0.001) compared with the late ToD group (P< 0.001). In summary, our study indicates that early ToD immunochemotherapy substantially improves PFS and OS and is associated with enhanced antitumor CD8+ T cell characteristics compared with late ToD treatment.
Time-of-day immunochemotherapy in non-small cell lung cancer: a randomized phase 3 trial
February 2, 2026
Retrospective studies suggest that early time-of-day (ToD) infusions of immunochemotherapy may improve efficacy. However, prospective randomized controlled trials are needed to validate it. In this randomized phase 3 LungTIME-C01 trial, 210 patients with treatment naive stage IIIC–IV non-small cell lung cancer (NSCLC) lacking driver mutations were randomly assigned in a 1:1 ratio to either an early or late ToD group, defined by the administration of the first four cycles of an anti-PD-1 agent before or after 15:00 h. The primary endpoint was progression-free survival (PFS), while secondary endpoints included overall survival (OS) and objective response rate (ORR). After a median follow-up of 28.7 months, the median PFS was 11.3 months (95% confidence interval (CI) = 9.2–13.4) in the early ToD group and 5.7 months (95% CI = 5.2–6.2) in the late ToD group, corresponding to a hazard ratio (HR) for earlier disease progression of 0.40 (95% CI = 0.29–0.55; P< 0.001). The median OS was 28.0 months (95% CI = not estimable (NE)–NE) in the early ToD group and 16.8 months (95% CI = 13.7–19.9) in the late ToD group, corresponding to an HR of an earlier death of 0.42 (95% CI = 0.29–0.60; P< 0.001). Treatment-related adverse events were consistent with the established safety profile, with no new safety signals observed. No significant differences in immune-related adverse events were observed between the two groups. Over the first four cycles, morning circulating CD8+ T cells increased in the early ToD group, whereas they declined in the late ToD group (P< 0.001). Furthermore, the ratio of activated (CD38+ HLA-DR+) versus exhausted (TIM-3+PD-1+) CD8+ T cells was higher in the early ToD group (P< 0.001) compared with the late ToD group (P< 0.001). In summary, our study indicates that early ToD immunochemotherapy substantially improves PFS and OS and is associated with enhanced antitumor CD8+ T cell characteristics compared with late ToD treatment.