Unsere Forschung entdecken
Bei TRR 418 eröffnen unsere Forschungen neue Einblicke in die circadiane Medizin. Diese Erkenntnisse werden in unseren Publikationen geteilt und bieten einen detaillierten Blick auf experimentelle, klinische und datenbasierte Studien, die zeigen, wie circadiane Rhythmen Gesundheit und Krankheit beeinflussen. Entdecken Sie unsere Publikationen, um die Evidenz, Methoden und Ideen hinter unserer Forschung kennenzulernen.
Time-of-day immunochemotherapy in non-small cell lung cancer: a randomized phase 3 trial
February 2, 2026
Retrospective studies suggest that early time-of-day (ToD) infusions of immunochemotherapy may improve efficacy. However, prospective randomized controlled trials are needed to validate it. In this randomized phase 3 LungTIME-C01 trial, 210 patients with treatment naive stage IIIC–IV non-small cell lung cancer (NSCLC) lacking driver mutations were randomly assigned in a 1:1 ratio to either an early or late ToD group, defined by the administration of the first four cycles of an anti-PD-1 agent before or after 15:00 h. The primary endpoint was progression-free survival (PFS), while secondary endpoints included overall survival (OS) and objective response rate (ORR). After a median follow-up of 28.7 months, the median PFS was 11.3 months (95% confidence interval (CI) = 9.2–13.4) in the early ToD group and 5.7 months (95% CI = 5.2–6.2) in the late ToD group, corresponding to a hazard ratio (HR) for earlier disease progression of 0.40 (95% CI = 0.29–0.55; P< 0.001). The median OS was 28.0 months (95% CI = not estimable (NE)–NE) in the early ToD group and 16.8 months (95% CI = 13.7–19.9) in the late ToD group, corresponding to an HR of an earlier death of 0.42 (95% CI = 0.29–0.60; P< 0.001). Treatment-related adverse events were consistent with the established safety profile, with no new safety signals observed. No significant differences in immune-related adverse events were observed between the two groups. Over the first four cycles, morning circulating CD8+ T cells increased in the early ToD group, whereas they declined in the late ToD group (P< 0.001). Furthermore, the ratio of activated (CD38+ HLA-DR+) versus exhausted (TIM-3+PD-1+) CD8+ T cells was higher in the early ToD group (P< 0.001) compared with the late ToD group (P< 0.001). In summary, our study indicates that early ToD immunochemotherapy substantially improves PFS and OS and is associated with enhanced antitumor CD8+ T cell characteristics compared with late ToD treatment.
Time-of-day immunochemotherapy in non-small cell lung cancer: a randomized phase 3 trial
February 2, 2026
Retrospective studies suggest that early time-of-day (ToD) infusions of immunochemotherapy may improve efficacy. However, prospective randomized controlled trials are needed to validate it. In this randomized phase 3 LungTIME-C01 trial, 210 patients with treatment naive stage IIIC–IV non-small cell lung cancer (NSCLC) lacking driver mutations were randomly assigned in a 1:1 ratio to either an early or late ToD group, defined by the administration of the first four cycles of an anti-PD-1 agent before or after 15:00 h. The primary endpoint was progression-free survival (PFS), while secondary endpoints included overall survival (OS) and objective response rate (ORR). After a median follow-up of 28.7 months, the median PFS was 11.3 months (95% confidence interval (CI) = 9.2–13.4) in the early ToD group and 5.7 months (95% CI = 5.2–6.2) in the late ToD group, corresponding to a hazard ratio (HR) for earlier disease progression of 0.40 (95% CI = 0.29–0.55; P< 0.001). The median OS was 28.0 months (95% CI = not estimable (NE)–NE) in the early ToD group and 16.8 months (95% CI = 13.7–19.9) in the late ToD group, corresponding to an HR of an earlier death of 0.42 (95% CI = 0.29–0.60; P< 0.001). Treatment-related adverse events were consistent with the established safety profile, with no new safety signals observed. No significant differences in immune-related adverse events were observed between the two groups. Over the first four cycles, morning circulating CD8+ T cells increased in the early ToD group, whereas they declined in the late ToD group (P< 0.001). Furthermore, the ratio of activated (CD38+ HLA-DR+) versus exhausted (TIM-3+PD-1+) CD8+ T cells was higher in the early ToD group (P< 0.001) compared with the late ToD group (P< 0.001). In summary, our study indicates that early ToD immunochemotherapy substantially improves PFS and OS and is associated with enhanced antitumor CD8+ T cell characteristics compared with late ToD treatment.
Detecting and exploiting the circadian clock in rheumatoid arthritis
August 23, 2023
Siska Wilantri, Hanna Grasshoff, Tanja Lange, Timo Gaber, Luciana Besedovsky, Frank Buttgereit
Over the past four decades, research on 24-h rhythms has yielded numerous remarkable findings, revealing their genetic, molecular, and physiological significance for immunity and various diseases. Thus, circadian rhythms are of fundamental importance to mammals, as their disruption and misalignment have been associated with many diseases and the abnormal functioning of many physiological processes. In this article, we provide a brief overview of the molecular regulation of 24-h rhythms, their importance for immunity, the deleterious effects of misalignment, the link between such pathological rhythms and rheumatoid arthritis (RA), and the potential exploitation of chronobiological rhythms for the chronotherapy of inflammatory autoimmune diseases, using RA as an example.
Insomnia increases the risk for specific autoimmune diseases: a large-scale retrospective cohort study
April 10, 2025
Sarah Stenger, Artem Vorobyev, Katja Bieber, Tanja Lange, Ralf J Ludwig , Jennifer E Hundt
Objective: The global rise of autoimmune diseases presents a significant medical challenge, with inadequate treatment options, high morbidity risks, and escalating healthcare costs. While the underlying mechanisms of autoimmune disease development are not fully understood, both genetic predispositions and lifestyle factors, particularly sleep, play critical roles. Insomnia and circadian rhythm sleep disorders not only impair sleep but also disrupt multi-organ interactions by dysregulating sympathetic nervous system activity, altering immune responses, and influencing neuroendocrine function. These disruptions can contribute to immune system dysregulation, increasing the risk of autoimmune disease development.
Methods: To assess the impact of impaired sleep on the risk of developing autoimmune diseases, a global population-based retrospective cohort study was conducted using electronic health records from the TriNetX US Global Collaborative Network, including 351,366 subjects in each propensity score matched group. Twenty autoimmune diseases were examined, and propensity score matching was employed to reduce bias. Three sensitivity analyses were conducted to test the robustness of the results.
Results: The study identified significantly increased risks for several autoimmune diseases associated with impaired sleep, likely mediated by dysregulated neuroimmune and autonomic interactions. Specifically, cutaneous lupus erythematosus [hazard ratio (HR) = 2.119; confidence interval (CI) 1.674-2.682; p < 0.0001], rheumatoid arthritis (HR = 1.404; CI 1.313-1.501; p < 0.0001), Sjögren syndrome (HR = 1.84; CI 1.64-2.066; p < 0.0001), and autoimmune thyroiditis (HR = 1.348; CI 1.246-1.458; p < 0.0001) showed significantly increased risks. No diseases demonstrated reduced risks, and 4 out of 20 tested diseases did not show significant HR increases in any analysis.
Conclusion: This study highlights the integral role of sleep in maintaining immune homeostasis through multi-organ interactions involving the autonomic nervous system, immune signalling pathways, and endocrine regulation. Disruptions in these systems due to chronic sleep impairment may predispose individuals to autoimmune diseases by altering inflammatory responses and immune tolerance. These findings underscore the necessity of recognizing and treating sleep disorders not only for general wellbeing but also as a potential strategy to mitigate the long-term risk of autoimmune disease development.
Keywords: TriNetX; autoimmune diseases; autoimmunity; insomnia; retrospective cohort study; sleep.
Time-of-day dependency of adoptive cell therapies
October 31, 2025
Constant Adriaan Tellinga, Roman Friedli, Federico Simonetta, Christoph Scheiermann
Adoptive cell therapies (ACTs), such as chimeric antigen receptor (CAR)-T cell therapy, have revolutionized cancer treatment, especially for hematological cancers. However, patient responses vary considerably. Emerging research reveals a striking influence of time of day (ToD) on ACT efficacy. Administering ACT during the early behavioral active phase enhances tumor control and reduces toxicity in preclinical models, an effect linked to the circadian clock. Latest clinical data also point to ToD effects in the cancer setting. In this opinion article we explore current insights and discuss the emerging underlying mechanisms. We propose that integrating ToD into clinical practice could represent a powerful yet easily implementable therapeutic regimen to improve efficacy and safety of ACT.
Circadian tumor infiltration and function of CD8+ T cells dictate immunotherapy efficacy
May 23, 2024
Chen Wang, Qun Zeng, Zeynep Melis Gül, Sisi Wang, Robert Pick, Phil Cheng, Ruben Bill, Yan Wu, Stefan Naulaerts, Coline Barnoud, Pei-Chun Hsueh, Sofie Hedlund Moller, Mara Cenerenti, Mengzhu Sun, Ziyang Su, Stéphane Jemelin, Volodymyr Petrenko, Charna Dibner, Stéphanie Hugues, Camilla Jandus, Zhongwu Li, Olivier Michielin, Ping-Chih Ho, Abhishek D Garg, Federico Simonetta, Mikaël J Pittet, Christoph Scheiermann
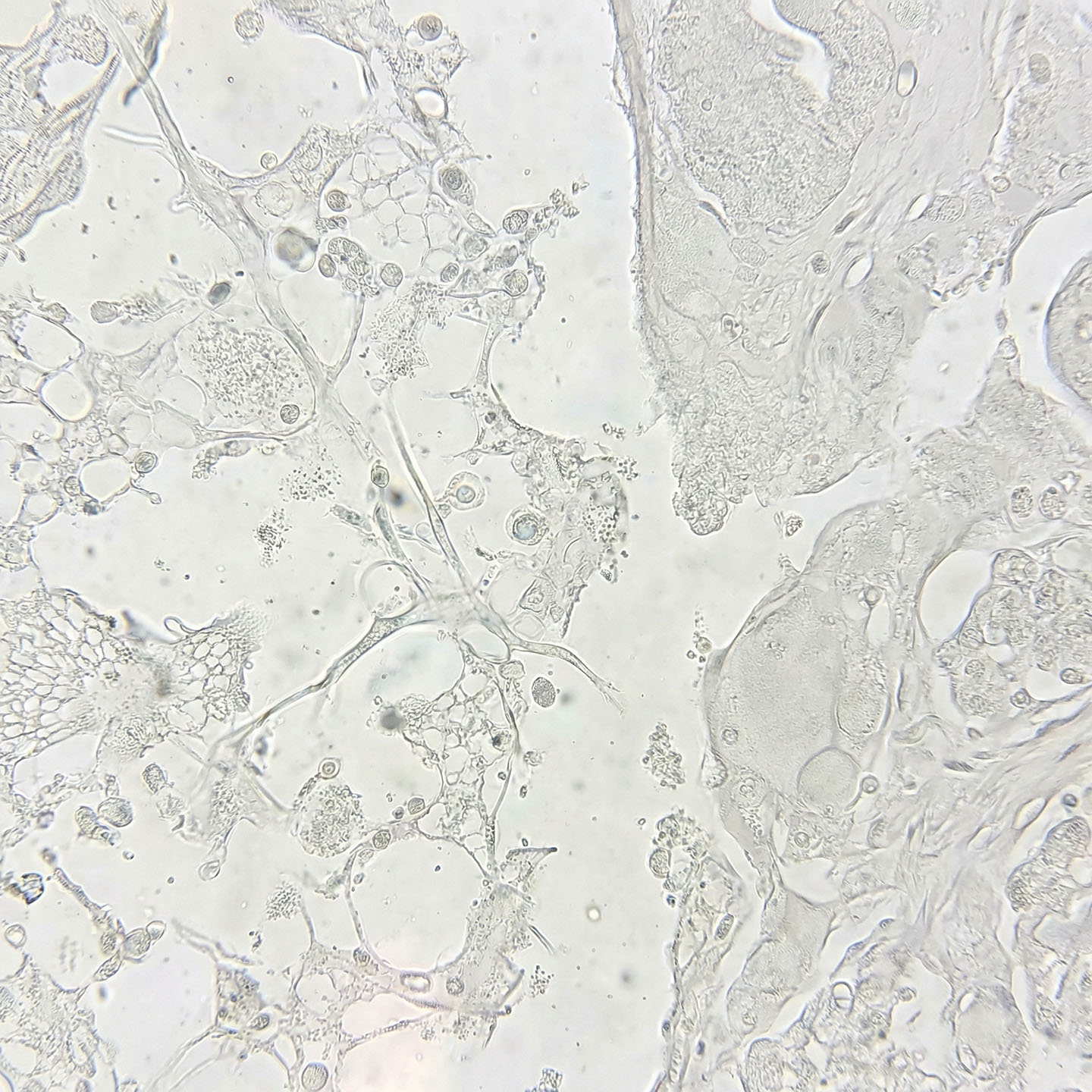
The quality and quantity of tumor-infiltrating lymphocytes, particularly CD8+ T cells, are important parameters for the control of tumor growth and response to immunotherapy. Here, we show in murine and human cancers that these parameters exhibit circadian oscillations, driven by both the endogenous circadian clock of leukocytes and rhythmic leukocyte infiltration, which depends on the circadian clock of endothelial cells in the tumor microenvironment. To harness these rhythms therapeutically, we demonstrate that efficacy of chimeric antigen receptor T cell therapy and immune checkpoint blockade can be improved by adjusting the time of treatment during the day. Furthermore, time-of-day-dependent T cell signatures in murine tumor models predict overall survival in patients with melanoma and correlate with response to anti-PD-1 therapy. Our data demonstrate the functional significance of circadian dynamics in the tumor microenvironment and suggest the importance of leveraging these features for improving future clinical trial design and patient care.
Circadian Rhythms in Anticancer Immunity: Mechanisms and Treatment Opportunities
June 30, 2024
Robert Pick, Chen Wang, Qun Zeng, Zeynep Melis Gül, Christoph Scheiermann
Circadian rhythms of approximately 24 h have emerged as important modulators of the immune system. These oscillations are important for mounting short-term, innate immune responses, but surprisingly also long-term, adaptive immune responses. Recent data indicate that they play a central role in antitumor immunity, in both mice and humans. In this review, we discuss the evolving literature on circadian antitumor immune responses and the underlying mechanisms that control them. We further provide an overview of circadian treatment regimens—chrono-immunotherapies—that harness time-of-day differences in immunity for optimal efficacy. Our aim is to provide an overview for researchers and clinicians alike, for a better understanding of the circadian immune system and how to best harness it for chronotherapeutic interventions. This knowledge is important for a better understanding of immune responses per se and could revolutionize the way we approach the treatment of cancer and a range of other diseases, ultimately improving clinical practice.
Impact of Intended Isocaloric Early versus Late Time-Restricted Eating on Plasma Lipidome in Women with Overweight or Obesity: Secondary Analysis of the ChronoFast Trial
November 4, 2025
Kristof Szekely, Mathias J Gerl, Beeke Peters, Julia Schwarz, Bettina Schuppelius, Markus Damm, Jorge R Soliz-Rueda, Ratika Sehgal, Michail Lazaratos, Christian Klose, Kai Simons, Andreas F H Pfeiffer, Annette Schürmann, Achim Kramer, Andreas Michalsen, Olga Pivovarova-Ramich
Time-restricted eating (TRE) is a promising strategy against metabolic disorders, but its effects on lipid metabolism remain controversial. The present research assesses and compares the impact of early (eTRE) versus late (lTRE) TRE on the plasma lipidomic profile. This is an exploratory outcome of the previously published randomized crossover trial, which examines 31 women with overweight or obesity who follow a two-week eTRE and a two-week lTRE in an intended isocaloric setting. Blood plasma and subcutaneous adipose tissue biopsies are analyzed using shotgun lipidomics and transcriptomics, respectively. Between interventions and within the lTRE, lipid species and classes, as well as enzyme activity indices, are not substantially changed. Within the eTRE, changes are observed for 103 lipid species, including a reduction of ceramide and phosphatidylcholine classes, and for the desaturation indices D5D, D6D, and D9D, as well as the elongation index ELOVL6. Combined analysis of plasma lipidome and adipose tissue reveals alterations in the glycerophospholipid pathway and in the expression of phospholipase enzymes PLB1, PLA2G6, and PLAG4B, dependent on TRE timing. These results suggest that eating timing during TRE may be crucial for remodeling the plasma lipidome and adipose tissue transcriptome and highlight the need of future lipidomic research in TRE.





